This section describes important activities that the HCRT may conduct during incident operations. These activities are relevant to the Healthcare Coalition regardless of whether the HCRT operates from a single physical location or via a distributed network.
3.5.1 HCRT “Leader” Function
As noted in Chapter 2, the HCRT position that performs the ICS “Command” function is more aptly referred to as an HCRT “Leader.” Key activities of this position during HCRT incident operations are described below.
Managing the Coalition’s emergency response
The HCRT Leader provides oversight and maintenance of the HCRT. Even during minimal HCRT activation, it is mandatory to designate the HCRT Leader. During initial activation, the Coalition Duty Officer transitions to the HCRT Leader position until he/she is relieved by another qualified individual. It is expected that other traditional ICS Command staff positions will be unassigned during most HCRT activations. The functions of these unstaffed positions are assumed by the HCRT Leader.
Important initial management actions include the following:
- Conduct an initial situation assessment.
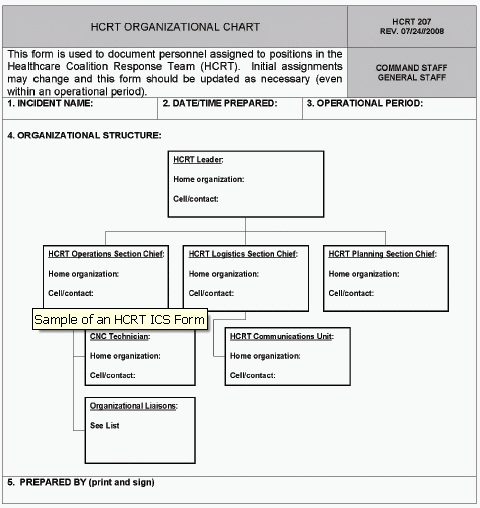
- Designate the structure of the HCRT and which positions will be staffed for the emergency. This should be documented and disseminated to Coalition member organizations, jurisdictional authorities (Tier 3), and other relevant response organizations (e.g., regional Healthcare Coalitions). This may be accomplished using an HCRT ICS Form 207 (Figure 3-2). Because the HCRT may evolve as the incident progresses, the structure should be updated as necessary. This level of transparency is critical to integrating the HCRT with other response entities.
- Establish initial objectives for the HCRT, then develop strategies and assign resources to achieve the objectives (Exhibit 3-7). Setting objectives for the HCRT, even if formal action planning is not conducted, fosters proactive team management and is important for overall response success.
| Figure 3-2. Example of an HCRT ICS Form 207 |
| Figure 3-2 shows a sample an HCRT ICS Form. This form is used to document personnel assigned to participate in the positions in the Healthcare Coalition Response Team. Initial assignments may change and this form should be updated as necessary (even within an operational period). The form contains a revision date and fields for the 1) Incident Name; 2) Date/Time Prepared; 3) Operational Period; 4) Organizational Structure; and 5) Prepared by. The organization chart is hierarchical and each box within the chart contains a space for the Position, Home Organization, and Cell/contact. The following positions are shown in the organizational structure: HCRT Leader is at the top. Below that cell are cells for HCRT Operations Section Chief, HCRT Logistics Section Chief, and HCRT Planning Section Chief. Under the HCRT Operations Section Chief is the CNC Technician and the Organizational Liasons. Under the HCRT Logistics Section Chief is the HCRT Communications Unit. |
|
|
Exhibit 3-7. Example incident and initial operational period objectives for the HCRT
Incident (Control) Objectives*
- Facilitate situational awareness for Healthcare Coalition member organizations
- Provide resource support to Coalition member organizations
- Facilitate coordination across participating Coalition organizations
- Facilitate the interface between jurisdictional authorities (Tier 3) and Coalition member organizations
Operational Period Objectives**
- Obtain and aggregate initial situation and resource assessments at individual healthcare organizations (Tier 1)
- Obtain initial situation and resource assessment from jurisdictional authorities (Tier 3) and regional sources
- Facilitate early, critical requests for assistance from impacted Coalition member organizations
- Obtain initial response strategies used by Coalition member organizations and assess these to identify potential conflicts or gaps
* Incident or control objective is the NIMS term for overall incident response goals and are not limited to any single operational period.
** Operational period objectives are more specific objectives (compared to incident or control objectives) for the organization to accomplish during a specific operational period, contributing towards achieving the incident objectives.
- Address safety issues for the Healthcare Coalition. If a Safety Officer is not assigned to the HCRT, this responsibility falls to the HCRT Leader. Safety issues for the Coalition include:
- Safety issues for HCRT personnel. These will depend on the type of incident, but may include the use of Personal Protective Equipment (PPE) during a contagious disease outbreak, or addressing irregular sleep cycles for staff who are working during a prolonged incident.
- Safety issues for Coalition member organizations. Collective issues related to response safety for Coalition member organizations should be addressed as well. However, this is typically addressed through the HCRT Operations Section, if established.
-
Address public information issues for the Healthcare Coalition. If a traditional Public Information Officer is not assigned to the HCRT, this responsibility falls to the HCRT Leader unless it is specifically assigned elsewhere (e.g., to a member of the Senior Policy Group). Public information issues for the Coalition may include:
- Media inquiries about the Coalition’s response during an emergency. It is important to identify an individual who can be interviewed and appropriately answer questions. Care must be taken to limit the message only to the Coalition’s activities.[3] The message should not attempt to address the activities occurring at individual healthcare organizations, unless requested to do so by those assets.
- Public information consistency across Coalition member organizations. The public message may need to be coordinated across healthcare organizations, if this is not specifically addressed by the relevant Jurisdictional Agency (Tier 3). This activity is best accomplished by the HCRT Operations Section (Section 3.5.2) with HCRT Leader oversight.
-
Conduct liaison activities. Depending on the complexity of the Healthcare Coalition and the demands of an incident, a liaison position may or may not be staffed in the HCRT during incident operations. Liaison activities, however, must still occur. An essential liaison activity is with the Jurisdictional Agency (Tier 3) or regional Jurisdictional Agencies (multiple Tier 3s). The HCRT should ensure the following:
- Appropriate information exchange with the jurisdictional response. This would commonly be the Tier 3 Medical or Public Health authority through the jurisdiction’s IMT, Emergency Support Function, or a Department Operations Center (e.g., Public Health Department Operations Center).
- Effective interface with other regional Healthcare Coalitions (other Tier 2s), if warranted.
- Interface with other response agencies that may be operating in parallel with the Jurisdictional Agency (Tier 3) that is directly supporting the Healthcare Coalition. For example, Federal Law Enforcement may be onsite at healthcare facilities to identify possible perpetrators among the incident victims. While formal interface should occur through the Jurisdictional Agency (Tier 3), direct liaison with the agency that is operating at the healthcare organization is beneficial.
Healthcare Coalition incident action planning
Incident Action Planning is an important activity for any response organization and is well described in NIMS.[4] Essentially, it is the methodology that response organizations use to proactively manage an incident by establishing incident objectives, developing strategies and tactics, and assigning resources to accomplish the objectives. It is meant to be an iterative process that continuously evaluates the success of the organization and determines whether objectives, strategies, and tactics need to be revised.
Incident action planning is often a formal process that involves a series of steps (including meetings) and documentation of the resultant action plan for dissemination.[5] Used appropriately, incident action planning can effectively coordinate the efforts of an organization and integrate those efforts with other response organizations. The following considerations related to incident action planning are relevant for the Healthcare Coalition response:
- When is formal action planning indicated for the Healthcare Coalition? Despite its benefits, formal action planning can be time and labor intensive. In addition, its intra-organizational benefits are most evident to organizations conducting tactical operations (as compared to coordinating entities like EOCs). Often, an HCRT may be able to address the benefits of action planning following the response objectives set for the Coalition and simply ensuring that appropriate information is disseminated (see Section 3.5.2). If resources are available to conduct action planning, the initial incident parameters that indicate formal action planning may be beneficial include:
-
An incident involves or impacts a significant number of Coalition member organizations
-
An incident is projected to be long in duration
-
Incident response appears exceptionally complex, such as after a large-scale bioterrorism incident.
Moreover, if the Coalition conducts formal action planning, much of the material that is required to develop the action plan may be available by incorporating elements of the individual action plans from Coalition member organizations (Tier 1).
- Who conducts formal action planning for the Healthcare Coalition? The Planning Section of the HCRT supervises the action planning process (see Section 3.5.2).
- What terminology should be used for Coalition action planning efforts? Traditional ICS dictates that there is only one “Incident Action Plan” for an incident. This is usually the responsibility of the incident command authority directly managing the primary incident. The HCRT may prefer to use “Healthcare Coalition Action Plan” to distinguish this planning from both incident command authorities and planning conducted by individual healthcare organizations.
- What is the scope of this formal HCRT action planning? This “Healthcare Coalition Action Plan” only addresses the scope of its activities in supporting Coalition member organizations and facilitating interface with jurisdictional authorities. To avoid confusion, the action plan should recognize activated entities such as the medical emergency support function in a local EOC or a Public Health Department Operations Center, and briefly describe how they interface.
Strategic planning and linkages to the Senior Policy Group
The HCRT Leader also manages the interface between the HCRT and the Senior Policy Group. This includes establishing a reporting cycle to provide situational awareness and HCRT performance information to the Senior Policy Group. In addition, the HCRT Leader should receive strategic or policy direction from the Senior Policy Group and supervise the implementation of the Senior Policy Group’s decisions.
3.5.2 Operations Section
The organization of the HCRT Operations Section may vary based on the overall complexity of the Coalition and the specific incident requirements. Positions are staffed according to the projected tasks for that incident. The following major functions within the Operations Section are presented for consideration.
Information processing
A key response function of the HCRT could be to collect and process incident information for Coalition member organizations. The type of information processed by the HCRT may vary based upon the type and duration of an incident and by the response objectives that each Coalition seeks to achieve. It can also involve reporting the same type of information (e.g., number of incident victims by specific categories) as a response evolves. In accordance with ICS guidance, the information is captured and archived by the HCRT Planning Section.
Examples of the information categories that could be collected from Coalition organizations (Tier 1) during an incident include:
- Situation reports on the operating status of healthcare organizations (Tier 1). This refers to both patient load and any hazard impact on the organization. Ideally, a template developed during preparedness will standardize information provided to the HCRT so it can be efficiently aggregated by the HCRT. The template should be somewhat flexible to capture specific information based on the incident. Common types of information that can be included in situation reports include:
- The number of incident patients and types of casualties. Pre-established patient categories may be used by all Healthcare Coalition members to standardize reports on the severity of patients receiving care at each facility (Exhibit 3-8). These categories may not match up exactly with categories used by EMS to triage and prioritize patients for transport, since they serve a different purpose (i.e., projecting resource need).
- Patient identifiers. This can be important for helping family members locate loved ones and for other tracking purposes (e.g., epidemiological investigation of an infectious disease outbreak). The Coalition must ensure that this information is captured in a manner that complies with relevant Health Insurance Portability and Accountability Act (HIPAA) and relevant State or local regulations.[6]
- Resource reports that describe the operating status at each healthcare organization. Coalition members may be affected directly by impacts on personnel and facilities or indirectly by impacts on utilities or road access. A collective picture of the impact on healthcare delivery may offer stark evidence that priority assistance is needed through mutual aid or the Jurisdiction Agency (Tier 3). Reporting this aggregated information to incident authorities and back to Coalition members enhances situational awareness.
Exhibit 3-8. Examples of patient categorizations
The Washington, D.C. Hospital Mutual Aid System established two simple patient categories (based upon projected resource needs) for use in reporting patient data during emergencies. The simplicity works well, especially during incidents where the exact needs of the individual patients may not be rapidly discernable. All hospitals understand and utilize the following categories when reporting.
- Major: patients expected to require admission and/or significant medical or hospital resources (e.g., operating room, critical care, extensive orthopedic intervention)
- Minor: patients expected to be treated and released, or who require very little medical or hospital resources.
Examples of the information that could be collected from the Jurisdictional Agency(s) or other response organizations to convey to Coalition members include:
- Situation reports describing the hazard impact on the community and public sector response assets.
- Transportation disruptions, projected length of utility loss, EMS issues, and 911 call volumes. These are valuable data for projecting resource need and identifying barriers to resource acquisition.
- Specific public health information, such as case definitions, during an infectious disease outbreak. Case definitions provided early during an incident can be critical in helping healthcare organizations collect and report epidemiological data. Rapid aggregation of these data and dissemination to Coalition members and relevant Public Health authorities may increase reporting compliance among Coalition member organizations.
- Other epidemiological data collected and analyzed by public health authorities to establish situational awareness. For example, data on work absenteeism or trends in the use of specific medications can be helpful to distribute to member organizations.
- Treatment protocols or guidelines promoting consistent patient care. These may be developed by expert personnel from Coalition member organizations using a consensus approach that incorporates public health recommendations. This is valuable not just for unique infectious diseases, but also when traditional medical issues must be addressed in non-traditional (alternate care) facilities. For example, general guidelines for the first 24 hours of care for burn patients who are being treated in non-burn facilities may facilitate appropriate medical care until additional assets can be mustered.
- The Incident Action Plan generated by the Jurisdictional Agency (Tier 3) with command authority for the incident response. Relevant information from the Incident Action Plan should be conveyed to Coalition members, such as the projected schedule for restoring utilities or clearing debris from roadways.
- Other updates, advisories, or alerts, such as an alert issued by the Centers for Disease Control and Prevention (CDC) or an “action plan” produced by a nearby Healthcare Coalition that may be dealing with a similar crisis.
What should the HCRT do with all of this information once it has been collected? This may vary from one Coalition to another, but some general next steps include:
- Information provided by Coalition member organizations (Tier 1) may be aggregated or summarized into a usable format, then disseminated back to members and the relevant Jurisdictional Agency(s) (Tier 3).
- The data may require some analysis to improve its value for recipients. For example, individual experts or a task force formed from within the Coalition organizations may briefly review and clarify the information before it is disseminated. Usually, the information can be distributed with minimal processing.
- The HCRT Planning Section should archive all information or data collected during HCRT response and recovery.
The Operations Section can also promote situational awareness by conducting a Situation Update teleconference. This can be particularly useful during complex or rapidly evolving incidents. The objective is to provide a balanced understanding of what has occurred so healthcare organizations can make informed decisions and anticipate future actions. Participants may include HCRT personnel, Organizational Liaisons from Coalition members (Tier 1), and representatives from relevant Jurisdictional Agencies (Tier 3) and other regional Healthcare Coalitions (Tier 2s). These calls generally include an incident summary followed by short briefings from jurisdictional authorities, heavily involved Coalition members, and informed experts invited by the HCRT to participate.
Resource support
Depending on the robustness of the Coalition, another key function of the Operations Section is to facilitate resource support for responding healthcare organizations (Tier 1). It is important to note that the Coalition only facilitates the established processes for resource support. It does not direct or control these activities between member organizations or between healthcare organizations and jurisdictional response entities (Tier 3) unless specifically delegated this authority from the proper Jurisdictional Agency. Coalition actions may entail the following:
- Facilitating mutual aid: The HCRT can notify Coalition member organizations when assistance is needed or anticipated by one or several Coalition members. The specific needs can be obtained from the requesting organization(s) and conveyed through the HCRT. Likewise, organizations that are able and willing to assist can respond through the HCRT so that offers of assistance can be rapidly aggregated. The HCRT can also facilitate the application of mutual aid instruments between organizations (see Chapters 4 and 7). Depending on how the Coalition has been constructed, assistance may include tracking resources shared between the organizations.[7] The HCRT must always keep Jurisdictional Agencies (Tier 3) managing the incident informed about resource requests and actions to meet the requests. Jurisdictional Agencies can then anticipate where additional assistance may be needed.
- Facilitating outside assistance: Requests for assistance to entities outside of the Coalition membership can be expedited by HCRT actions. Requests from member organizations may be rapidly aggregated and transmitted to the Jurisdictional Agency (Tier 3). When a Healthcare Coalition crosses jurisdictional boundaries (e.g., the Coalition covers organizations in adjoining cities, counties, or regions), the Coalition must coordinate these requests through the respective jurisdictional authorities (Tier 3).
- Facilitating requests to other regional Coalitions, whether assets are being sent to or received from these entities. Keeping relevant Jurisdictional Agency(s) informed of the situation is critical.
- Facilitating the placement of specialty patients: For example, after an incident with multiple burn patients, initial care can be started at local healthcare facilities while the HCRT assists hospitals and jurisdictional authorities (Tier 3) in locating burn beds in the region, State, or country. This promotes the placement of patients via a medically sound priority scheme.
- Facilitating resource support from Coalition organizations to jurisdictional authorities (Tier 3): During incidents in which the jurisdictional response entities require healthcare assistance, such as a mass biological exposure of first responders, the HCRT Operations Section can facilitate assistance from available healthcare organizations.
Facilitating a coordinated response among healthcare organizations
Certain incidents highlight the need for consistency in response actions across Coalition member organizations. This is often necessary during the response to an unusual infectious or toxic agent (evaluation and treatment protocols, case reporting, etc.). The HCRT may promote consistency across “Healthcare Organization Action Plans” by facilitating brief discussions among Coalition members and the sharing of draft action planning products as the incident evolves. Any perceived or actual conflict in the intended response actions of the organizations can then be addressed directly by the involved entities, either by producing a joint explanation for the perceived conflict or by resolving the conflicting material before it is distributed or put into action. This is a facilitating function only and does not subvert the incident command authority of Jurisdictional Agencies or the autonomy of Coalition member organizations.
Methodology
The HCRT Operations Section may establish an iterative information sharing process to facilitate coordination between the incident management elements within the responding healthcare organizations. Consistent with the ICS “management by objectives” approach, this process may entail:
- An operational period (i.e., the time during which one Coalition Action Plan is applicable) is established along with a reporting schedule for Coalition member organizations.
- Elements of individual organization action plans, such as patient screening protocols, may be collected and compared. Any major conflicting strategies are identified (see Exhibit 3-9).
- A response coordination teleconference may be conducted. Any differences in response tactics or actions between healthcare organizations can be identified and discussed. In this manner, healthcare providers will be better prepared to address issues related to consistency in the healthcare services provided to incident patients.
- An aggregated report of specific items from healthcare organization action plans may be developed. The aggregated report is forwarded to relevant Jurisdictional Agency(s) (Tier 3) while simultaneously being returned to member organizations.
Exhibit 3-9. Example of the importance of coordinating strategies of individual healthcare organizations
During the anthrax attacks in 2001, hospitals in the Washington, D.C. area did not initially coordinate their efforts for screening and evaluating potentially exposed patients. For example, some hospitals conducted nasal swabbing as a diagnostic test despite evidence that it was useful only for epidemiological purposes. The resultant confusion led to “hospital shopping” by some patients until they found a facility that would conduct the test for them. Criteria to determine which patients received prophylaxis also varied between health facilities. The lack of a consistent approach further increased the anxiety of the public and led to speculation of “class disparities” in evaluation and treatment recommendations.
Authors’ observations; Gursky E, Inglesby TV, and O’Toole T. “Anthrax 2001: Observations on the Medical and Public Health Response.” Biosecurity and Bioterrorism: Biodefense Strategy, Practice, and Science, Volume 1, (2003).
The information contained in the Coalition members’ action plans will help formulate the Healthcare Coalition’s Action Plan. A consensus among the organizations may be reached for incident and operational period objectives, strategies, and major tactics. While specific tactics may vary somewhat at each organization, it is ideal to have general consistency across the Coalition.
If the Coalition elects not to conduct formal action planning, it may still be valuable to establish regular reporting times and data categories for member organizations in order to maintain situational awareness and strategy consistency. In addition, the Coalition may want to conduct the equivalent of an operations briefing at least once during each operational period. Updates on the incident and the HCRT’s response actions can be provided. Participants should include the organizational liaisons to the HCRT and liaisons from relevant Jurisdictional Agencies (Tier 3).
Requirements
For the Healthcare Coalition to support these activities it must have the ability to effectively send and receive information from Coalition member organizations (Tier 1) and Jurisdictional Agencies (Tier 3). The HCRT should be able to link its member organizations in real-time for teleconferences, web-based information sharing, and other activities. Ideally, these communication methods should be available independent of Jurisdictional Agencies or any Coalition organization to ensure they are available to the Coalition during any type of major emergency.
3.5.3 HCRT: Support Sections
If the HCRT is structured according to ICS principles, staffing of the various support functions (Logistics, Planning, Administration/Finance) may be necessary depending on the incident parameters and the robustness of the Coalition. To keep the Coalition as lean as possible, these functions should only be staffed as necessary for the specific emergency (see Section 2.3).
3.5.4 Healthcare Coalition Senior Policy Group
In many emergencies, the services of the Healthcare Coalition Senior Policy Group may not be needed. However, when their services are needed, the Senior Policy Group will typically meet via teleconferencing. These meetings should be managed by the HCRT Leader to keep them focused and concise. A record should be kept of the discussions and any directives from the proceedings should be disseminated to the Coalition member organizations.
The Coalition should define a process during preparedness planning for how the Senior Policy Group will make decisions during an emergency. Personnel staffing the Senior Policy Group should be trained and exercised on this decision process. For example, a majority vote may be adequate in most cases; however, if there are multiple organizations within the Coalition owned by one parent company, then consideration may be given to “weighted” votes to maintain fairness across the Coalition. The Senior Policy Group should have access to technical experts within the Coalition (Exhibit 3-10) to help them make informed decisions. At the invitation of the Senior Policy Group, representatives from Public Health, EMS, and other local Jurisdictional Agencies (Tier 3) may serve in an advisory capacity.
Exhibit 3-10. An example of a notional Senior Policy Group decision
During response to the intentional release of anthrax, the Strategic National Stockpile has been distributed according to pre-established protocols within the jurisdiction. However, due to the pattern of release, Hospital X has been screening more patients than the larger Hospital Y. A request for re-distributing pharmaceuticals has met resistance by some Coalition member organizations. To resolve the discord, an emergency meeting of the Senior Policy Group is conducted.
During the meeting, which is facilitated by the HCRT Leader, a decision is made to redistribute the medications based on an agreed-upon projection of need. A follow-up Senior Policy Group meeting is scheduled for further review and distribution revision, if indicated.
- Global assessments of the situation are the role of the Public Information Officer from the relevant Jurisdictional Agency.
- Department of Homeland Security, National Incident Management System (NIMS), December 18, 2008. Available at: http://www.fema.gov/emergency/nims/.
- Commonly known as “ICS forms,” there are numbered document templates that are used to form the basic Incident Action Plan. ICS forms 202, 203, 204, 205, and 206 form the core components of the Incident Action Plan.
- Healthcare Coalitions may find it helpful to work closely with local and State public health authorities to formally address these concerns.
- Resource tracking may occur at the healthcare organization level; however, the HCRT should still confirm that the resource tracking is actually occurring.
<<Previous - Return to Top - Next>>
