The mechanisms that the HCRT uses to interface with Coalition member organizations (Tier 1) and the relevant Jurisdictional Agency(s) (Tier 3) during emergency response should be designed to maximize efficiency. While multiple examples are presented in this chapter, they are not intended to be prescriptive. They are provided to stimulate discussion among those responsible for developing a Coalition.
4.1.1 Response Strategies for Supporting Coalition Member Organizations (Tier 1)
In Section 2.1.1, candidate incident response and recovery objectives were presented for the Healthcare Coalition. If these objectives are adopted by a Coalition, then the strategies used to achieve them can be grouped according to the following categories:
- Promote situational awareness and consistent response actions among Coalition member organizations by facilitating information sharing.[1]
- Represent the collective interests of the Coalition member organizations in addressing issues with incident command and jurisdictional authorities (Tier 3).
- Facilitate resource support to Coalition organizations through mutual aid and other assistance mechanisms.
- Enhance support to Coalition member organizations from the Jurisdictional Agency (Tier 3) directly or from other entities (e.g., State or Federal government) through the Jurisdictional Agency.
Examples of response strategies that a Healthcare Coalition may incorporate into its EOP are provided below.
Promoting situational awareness and consistent response actions among Healthcare Coalition member organizations
The information processing function of the HCRT plays a key role in providing situational awareness among Coalition members. As an extension of this strategy, the HCRT can also promote consistency in response actions among its member organizations without impinging on their independent decision-making authority. The Coalition can achieve this support through the following actions:
- Collecting, compiling, and reporting situation updates and other data from Coalition members. Reported data may include how the hazard has affected each healthcare organization in terms of patient volume, patient types, or direct impact on the healthcare organization itself. Information collected and disseminated can also include how Coalition members are responding.
- Facilitating patient tracking for Coalition member organizations and providing this information back to healthcare organizations so they can assist families searching for loved ones.
- Collecting, compiling, and reporting information about each Coalition member’s response strategy.
- Collecting (from Public Health authorities or subject matter experts) and disseminating recommendations related to specific response actions for unusual patient cases. These recommendations could include information related to changes in the understanding of a disease or injury pattern or protocols for the evaluation or treatment of incident patients. These efforts require close coordination with Public Health authorities.[2]
- Promoting consistent public messaging for Coalition member organizations. This can be achieved, in part, by disseminating public information guidance from the Jurisdictional Agency (Tier 3), which has lead responsibility for public information. As discussed in Chapter 3, it may entail convening individuals from member organizations to promote consistency of public messages. The Coalition may also monitor the media for erroneous or alarming messages that could impact the public perception of the healthcare response.
Representing the collective interests of Coalition members to the Jurisdictional Agency (Tier 3)
The HCRT can represent Coalition members in their interactions with the Jurisdictional Agency (Tier 3) during response and recovery. Examples of activities the Coalition could engage in include:
Addressing public sector actions that might adversely impact healthcare organizations: Public safety, public health, and other agencies may implement response tactics that inadvertently compromise operations at healthcare organizations. For example, roadblocks used to secure an area during a mass gathering can hinder healthcare personnel from reporting to their workstations. The HCRT can bring these types of issues to the attention of the jurisdictional authorities in an effort to resolve them.
Promoting financial support to healthcare organizations for response services and expenses: Because of the fiscal environment in which many healthcare organizations operate, they are especially vulnerable to interruptions in reimbursement for services, increased expenses related to medical surge, or other service obligations, such as mass decontamination. These activities often do not have a clear mechanism to recoup expenses, especially when the specific patient population is not insured. The Healthcare Coalition, working with its members and jurisdictional authorities, can facilitate solutions in conjunction with third party payers and government funding sources. Potential issues that the Coalition may address include:
- Payment for emergency response services that do not have a billing code. As noted above, some emergency actions may not have assigned billing codes, but may generate significant costs for the Coalition member organizations (e.g., decontamination, preparations for a large security event). The HCRT can facilitate meetings between Coalition member organizations and the appropriate authorities to promote fair reimbursement for these services.
- Payment for services provided in “non-participating” and “non-traditional” healthcare settings. Third party payers may have contracts for services that are provided only at certain preferred (“participating”) healthcare organizations, or facilities with a designated level of service (e.g., pediatric care at a hospital licensed and accredited for pediatric services). During emergency response and recovery, it may be helpful to modify these restrictions when the healthcare system is severely challenged. The HCRT can facilitate meetings to bring this issue to the attention of the appropriate authorities to seek resolution.
Addressing uneven patient distribution: Given the likely influx of victim “walk-ins” during a mass casualty incident and the potential for a direct hazard impact on healthcare delivery, strategies for patient distribution may need to be adjusted in real-time. The HCRT can assist with this by collating data (status reports) from individual healthcare organizations and transmitting the data to EMS or other authorities managing patient distribution. In addition, returning the aggregate data to Coalition member organizations enables them to anticipate response actions and develop contingency plans.
Facilitating mutual aid and other resource support between Coalition member organizations
As noted earlier, Healthcare Coalitions can serve an important role in facilitating mutual aid and other resource support between healthcare organizations. Key roles for the Coalition are described below.
Facilitating requests for and offers of assistance: The HCRT can receive and disseminate requests for assistance; receive offers of assistance from all legitimate sources (other Coalition members, jurisdictional authorities, etc.) and convey them to the impacted organization; connect the organizations offering assistance to the requesting organization; assist the requesting organization with determining which resources are best suited to fulfill the need;[3] and transmit all mutual aid requests and related actions to the relevant Jurisdictional Agency(s) (Tier 3). In some instances, the most important assistance may be to screen the deluge of assistance offers (at the request of the impacted organizations) and convey only those offers relevant to the described needs, thus lightening the burden on facility managers at the impacted organizations.
The process for requesting and offering assistance should be based on a written instrument that is adopted by all Coalition members during preparedness planning (see Section 7.3). This enables the HCRT to assist with the resource sharing process while avoiding any command decision-making role.
Trouble-shooting issues related to mutual aid: Despite the best intentions, conflicts related to resource support may arise between Coalition members. The Coalition may establish procedures for resolving these conflicts. In some situations, the Coalition’s Senior Policy Group may become involved. However, the Coalition only facilitates the interface between the involved parties; it typically has no authority to be the arbiter or determine a resolution.
Facilitating resource support from jurisdictional authorities
The HCRT may facilitate external resource requests and assistance for its member organizations when mutual aid from within the Coalition is unavailable or insufficient. Much of this is conducted through a process similar to the facilitation of mutual aid between Coalition members. Specific concepts for consideration are described below.
Coordination of resource requests: When resources are needed by multiple healthcare organizations simultaneously, the requests can be processed more efficiently if they are received by the Jurisdictional Agency(s) (Tier 3) through one source (i.e., the HCRT). The HCRT can provide a “needs picture” to the Jurisdictional Agency(s). The HCRT can also standardize the format and wording of requests to improve the accuracy of their interpretation by the Jurisdictional Agency (Tier 3) or by State (Tier 4) or Federal officials (Tier 6) who receive requests through the Jurisdictional Agency.
Distribution of resource assistance: The Healthcare Coalition can promote a “level playing field” for its members by facilitating how resources are best distributed to meet patient need. For example, the HCRT might hold a teleconference between organizations that are requesting the same scarce resource (e.g., ventilators) from a medical equipment cache. The HCRT can help the requesting organizations reach an agreement on the most appropriate way to distribute the scarce resource. The Senior Policy Group may be asked to assist with any particularly contentious or controversial allocation decisions.
Emergency patient transfer out of the area: If patient transfers are required outside of the Coalition’s geographic area, the Healthcare Coalition may support its member organizations through direct interface with the Jurisdictional Agency (Tier 3). The HCRT may serve as a coordinating point in conjunction with the Jurisdictional Agency as it prioritizes and allocates these transfers.
4.1.2 The Emergency Response Relationship between Tier 1 and Tier 2
The healthcare organizations that participate in the Healthcare Coalition must have robust incident management capabilities within their respective institutions to effectively interface with the HCRT.
The management element that is responsible for emergency response at a healthcare organization is commonly called an Incident Management Team (IMT). How the healthcare facility’s IMT interfaces with the HCRT should be clearly defined using ICS principles and terminology. For example, the position within the healthcare organization’s IMT that interfaces with the HCRT would be the organization’s Liaison Officer. If that position is not staffed, the responsibility falls to the IMT Leader (e.g., hospital incident commander) unless delegated elsewhere. It is recommended that Coalition members identify this individual to the HCRT at the start of any incident. Personnel assigned to this position must be prepared to:
- Participate in Healthcare Coalition meetings or teleconferences and provide any information that is requested by the HCRT
- Disseminate information provided by the HCRT to appropriate decision makers within their own organization
- Participate in their respective organization’s action planning in order to convey relevant information received from the HCRT, such as requests for resource support
- Notify the HCRT when being relieved of duties and provide the name and contact information for his/her replacement.
In some Healthcare Coalitions, the Organizational Liaisons to the HCRT could perform additional tasks during incident response. One example might be forming a task force (under the HCRT Operations Section) to achieve consensus on patient evaluation and treatment protocols.
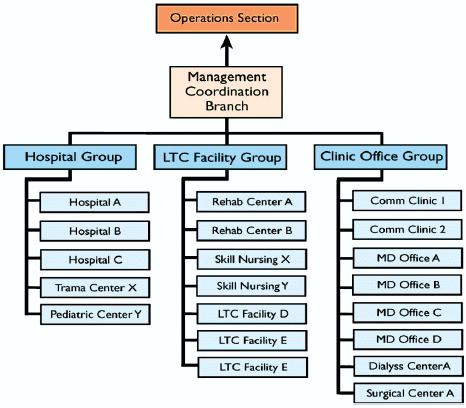
The formal interface between the HCRT and Coalition member organizations generally occurs through the HCRT Operations Section if one is established (otherwise, the interface is directly with the HCRT Leader). This linkage with the HCRT Operations Section may be directly with the Operations Section Chief for a small Coalition or when addressing a straightforward incident. During complex incidents, the reporting relationship could be subdivided to facilitate the reporting requirements. For example, the HCRT could consider utilizing branches, divisions, or groups to assist with an orderly process. These considerations are entirely up to the Coalition in question and may vary from incident to incident. An example reporting relationship for a robust Coalition responding to a complex incident is shown in Figure 4-1.
|
Figure 4-1. Structure for the interface between the Healthcare Coalition and participating healthcare organizations based on functional groupings
|
| Figure 4-1 depicts an example of a reporting relationship for a robust Coalition responding to a complex incident. At the top of this organizational structure is the Operations Section. Underneath the Operations section is the Management Coordination Branch. There are three branches under the Management Coordination Branch: Hospital Group, LTC Facility Group, and Clinic Office Group. There are Hospitals, a Trauma Center, and a Pediatric Center under the Hospital Group. There are Rehab Centers, Skill Nursing, and LTC Facilities under the LTC Facility Group. There are Comm Clinics, MD Offfices, a Dialysis Center, and a Surgical Center under the Clinical Office group. |
|
|
Smaller Coalition members and those with minimal administrative capabilities (e.g., physician office, community health centers) may interface with the HCRT in various fashions (see Chapter 5). Typically, these arrangements are limited to receiving and sharing information.
- It is anticipated that this will be the most frequent activity that any Coalition will be engaged in during emergency response.
- At the same time, the Coalition’s information collection efforts from member organizations could assist public health authorities with rapid epidemiological investigations and disease characterizations.
- The term “resource” should not be limited only to personnel, supplies, or facilities directly related to patient care. Healthcare organizations may require assistance with management services, technical advice, infrastructure support (e.g., engineering, security) or supplies for continuity of operations (e.g., water, food).
<<Previous - Return to Top - Next>>
